This is our annual report which provides information on how we help and support Calderdale residents who need to draw on care and support to live their 'largest life'. We also work with people and communities to prevent, delay and reduce the need for care and support to maximise people's independence, choice and control.
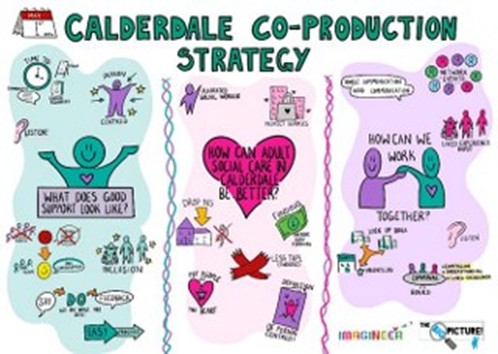
We are committed to co-production and to listening to the voices of people with lived experience. We are working alongside local groups, people who draw on care and support and their families and carers to continually improve and develop services. In 2024, we collaborated with a number of people and groups to develop our Co-production Strategy.
The views of the co-production group have influenced the update of this Local Account.
We have a new vision for Adult Services which has been co-produced with our staff in Adult Services and Well-being. This embodies our culture and commitment to putting people and equality at the heart of everything that we do.
Text version of the above image:
People are supported to live their largest life. We will always be kind and compassionate, creative and bold in helping people achieve their hopes and dreams. People are at the heart of all we do and they will feel valued and have an equal voice in their care and support. We will always respect people’s strengths and support them to be connected to their communities.
The Local Account sets out:
- How you can access advice and information or other support, in a way that is personal to you.
- How you can tell us what you think about our performance.
- Some of the things that we have done well.
- Some of the things we need to focus on and improve.
- Our plans for the future.
Our ambition is to support you to:
- Build on your strengths, whatever your abilities.
- Be as independent as you can, for as long as you can.
- Play an active part in your community.
- Lead the largest life you can by being in control of the things that are important to you.
There is a glossary at the end of this document which explains the terms used in the Local Account.
If you have any comments about this Local Account, please do let us know. Details of how to do this are in the Tell us what you think section of this document.
Thank you.
Cath Gormally, Director for Adults Health and Wellbeing.
What adult social care is
It can offer a range of support and advice to:
- people who may need care and support;
- carers;
- and family members.
This can be from us or organisations that we can put you in touch with. It can help you to continue to look after yourself, stay safe and live the life that you want.
We will support you:
- By listening to you to understand:
- what you need help and support with in your daily life;
- and what outcomes you want to achieve.
- To have as much choice and control and be as independent as possible.
- By making sure that the decisions you make, help you to stay safe and well.
- To connect to your community, have the right support networks and feel connected to people who are important to you.
If you need support, please email: gatewaytocare@calderdale.gov.uk to discuss how best to meet your needs. We will also help to make sure that you do not pay more for support than you can afford.
How to get information and advice
There is a range of support available from us or other organisations that we can put you in touch with. If you feel we could help, please contact Gateway:
- Online: Contact webform.
- Email: gatewaytocare@calderdale.gov.uk.
- In person at a Better Lives Hub. For times, dates and venues, please visit: Better Lives Hubs.
- Phone: (01422) 393000:
- Monday to Thursday from 8.45am to 5pm.
- Fridays from 8.45am to 4.30pm.
- Please note: Closed on Saturdays, Sundays and public holidays.
For social care needs causing risk or concern outside the hours above, phone the Emergency Duty Team: (01422) 288000.
Online
Find out how and when we can support you and your family's social care needs, see: Adult social care services.
For information, advice and guidance about health and wellbeing, visit: CalderConnect - Adults Community Information and Directory. This connects people to support and opportunities in their community and brings together what is happening in Calderdale.
It covers:
- groups;
- activities;
- organisations;
- buildings;
- and spaces.
It also allows you to browse/buy products and services that might be helpful for you.
If you need help to explain things
Gateway is there to answer your questions or concerns. If they cannot do this directly, they can put you in touch with advocacy or peer support. For example, if you are living with Autism, mental health conditions or have a learning disability.
There are also groups that can help you or your carers that offer friendship, support and ways to cope.
Useful links
- Calderdale Healthy Minds. Provide high-quality mental health services to people and families in Calderdale.
- Calderdale - Vita (Vita Health Group).
- Calderdale Advocacy Service (Cloverleaf). These help people to understand and uphold their rights.
- Lead the Way. A service for people with learning disabilities.
- Calderdale Self-Advocacy Network (Cloverleaf). This has groups for adults with a learning disability that live in Calderdale.
- Healthwatch Calderdale. An advice and information service for social care and NHS support. They will help you to have your say about the support that you get.
How to get early help
If you need support, we may be able to help you in your own home with things like:
- Increase your confidence.
- Provide technology to keep you safe, like care alarms or door sensors.
- Introduce you to community activities in your area.
- Support you to be physically active.
- Improve your mobility and prevent falls.
- Everyday tasks, such as making a meal, cup of tea, medication prompts and more.
- Advice, equipment or changes to help reduce the impact of illness/disability on your health, well-being and independence.
- Support you to gain employment.
- Support you with housing issues.
You can also get help from social care staff through our out of hours team.
Other early or preventative support that you can get in your home
Depending on your situation, the sort of things that might help you include:
Care Line System and responder service. Linked to a responder centre where someone can arrange help or contact your family and friends, should you need support.
- Fall detectors.
- Door, bed and chair sensors.
- Smoke or carbon monoxide detectors.
Medication dispensers/Pivitols. These make taking medication easier or remind you when to take it.
Tracking systems. These can help if you care for someone with dementia who goes "purposeful walking" at times.
The Reablement Team. They can support you for up to six weeks. This can be to help you to regain your independence while:
- you recover from an illness or injury;
- or if you have been diagnosed with dementia.
They can also help if you just need a bit of extra help to continue living at home.
Urgent Community Support. They can support you to avoid having to go into hospital or on discharge from hospital. This is a multi-disciplinary team health and social care team that can provide a wraparound service to assist you in recovery from an illness. They can then provide you with advice and information or connect you to ongoing care services if needed.
Link into Calderdale (LinC). Initial contacts come into Gateway through phone lines, emails and the online Wellbeing Contact Form. Gateway social workers will provide a rapid, on-the-day response to people presenting in an urgent and crisis situation who cannot safely wait any longer and are not allocated to a social worker.
Most people are helped to resolve the issues they have contacted us about at this point. This includes for OT support with equipment, aids and assistive technology.
If the person needs more support, our LinC team works with them for up to six weeks and will:
- Focus on making the situation stable.
- Identify short and medium term goals.
- Connect people with community resources to maximise independence and social support.
Our 8Ps approach makes sure that we support the whole person.
Better Lives Hub. The Better Lives Hubs are bringing face to face social care support into your community. They are a first point of contact, providing help and advice. Located in various community hubs within Brighouse, Elland, Halifax and Mixenden.
No appointment is needed, just drop in. All people over 18 are welcome.
Drop in with any questions about care and support from a range of professionals including social care advisors, care coordinators, social workers, nurses and occupational therapists.
This is to help you to:
- Find the services you need.
- Arrange the care you need.
- Get advice and support.
For more about these services, please contact Gateway:
- Phone: (01422) 393000.
- Email: gatewaytocare@calderdale.gov.uk.
- Website: Contact webform.
How to get support
Do you or someone you care for need information or advice? Do you need some support to keep living at home?
Our aim is to work with you to get the best outcome for you as quickly as possible.
To find out what support is available, please contact our Gateway team. Our advisor will take some basic details from you and agree with you the next steps. They may be able to help you there and then.
If they cannot, they will arrange for someone to contact you to discuss your needs and outcomes further. They may find you options in your community at little or no cost to keep you independent. It could mean that the support you require may need to be ongoing. If so, this would involve having an assessment.
What an assessment is
This is where a social worker, service co-ordinator or occupational therapist will have a conversation with you about any social care support that you might need. They will discuss things with you, such as:
- What is important to you and what you want to achieve.
- Your strengths and support networks.
- Your needs and well-being.
- The things that matter to you.
- What your your desired outcomes are.
- How much you will pay, if anything. For more about this, please see: Paying for your care and support.
After the assessment, we will see if any of your needs are eligible for care and support from us. If they are, we will work out how your well-being can be maintained and agree a plan with you.
For more details about the way we work or about social care needs, please see: Care Act 2014.
What a Well-being Plan is
This is a document that we will complete with you. It sets out the detail of your desired outcomes and how they will be achieved.
What type of services you can access after your assessment
Some examples of support in your own home include:
Equipment and changes to your home environment. We can provide advice and a range of equipment or adaptations to your home which will help reduce the impact of illness/ disabilities on your health, wellbeing and independence. These would also help those that help care for you continue to do so in a safe way. For example, a piece of equipment to help you get in the bath or a stair lift. We can also carry out moving and handling assessments, which focus on keeping your dignity, choice and control.
Mobile response and monitoring service. We can provide you with equipment and sensors that are connected to a mobile response call centre. Should you need assistance they can send someone to your home to help you or alert family and friends and inform them that you need assistance. This support can help you (or those you care for) to live safely and independently at home.
Floating support. A range of help and support for people over 60 years old, in your own home or tenancy. This will focus on you being able to keep your home and independence.
Home care. There are a range of care providers that we approve who can visit you at home and help you to stay independent. This can be provided several times a day if you need it.
Carers can support with personal care, help you to prepare meals and look after your home.
Social care can be accessed via a direct payment. This gives greater choice in terms of when, where and how you get the support you need.
Day opportunities. These provide:
- A range of opportunities and activities across Calderdale to support you.
- Health and social care support for older people or adults with a learning disability. (This includes complex needs, like dementia, autism or physical health needs.)
- Social, leisure and employment opportunities to meet your outcomes and promote your well-being.
Shared Lives. Provides focussed support in a range of home settings. This can be for a short time or longer period. We will work with you to match you to the carer who is best able to meet your needs. For more about this, please see: Adult placement schemes.
Supported living. There is a wide range of accommodation and support available. This ranges from independent apartments to shared houses and the support provided varies according to tenants' needs.
We work with a wide range of housing and support providers to make sure that this can meet the full range of tenants’ needs. We continue to review it and work with landlords to develop new accommodation of a high standard that is adaptable and responsive to changing needs.
Extra care. Provides accommodation with shared communal facilities and on-site support. Tenants have their own front door, but can access on-site support, based on their individual needs.
There are five schemes in Calderdale. This includes Railway Bridge in Brighouse, which provides specialist accommodation for people with dementia. One scheme is closed for major works to be done and re-opens in 2025.
Care homes. There are a number of options for 24-hour care, such as:
- Residential care, which gives help with all aspects of personal care.
- Nursing care, where there is always a qualified nurse on duty, for those who have more complex needs.
- Residential and nursing homes that offer specialist support to people with dementia.
Short stay provision provides accommodation for people who need on-going support following a hospital admission or can be used to offer a short break to family carers.
There are residential and nursing homes that specialise in supporting younger adults with learning disabilities. There are also homes that specialise in supporting older people.
Arranging and paying for care and support
We make sure that you do not pay more for support than you can afford. For the most up to date charging information, please see: Paying for your care and support.
If you want to get your own care and support
We will tell you about something called a Personal Budget. This is the amount of money that we work out with you that will cover the cost of your social care support. You can ask for this to be paid as a Direct Payment.
Direct Payments: This is a way you can receive money from the Council, if you are eligible. This is to help you pay for the care and support you need.
- Choose this to have more control over the services you use and where you get them from.
- You can spend this on any services that are legal, keep you safe/healthy and meet your eligible needs.
- We will pay the money into your bank or building society account.
Please note: Direct payments do not count as income and will not affect your benefits.
If you cannot make decisions for yourself
Someone, who is interested in your welfare, can support you. We will work with them to agree on how your identified outcomes should be met. We will do all we can to achieve this.
If you or someone you care for has a learning disability
- Lead the Way. A community advice and support service for you and your carers.
- Calderdale Advocacy Service (Cloverleaf). A self-advocacy service to help you make decisions and express your concerns.
If you want to get a job, there are some ways we can help you. These includes:
- College Placements. 5-day support is available for people moving between children's and adults' services, in partnership with the local adult education provider.
- Supported Internships and Project Search in partnership with the NHS. This offers internships to young people in partnership with the local hospital. There are up to twelve internships each year in this well-established scheme that has provided successful employment opportunities for young people.
If you have care and support needs we can help you to find accommodation to be as Independent as possible.
There is a wide range of support available, from independent apartments, to supported living and 24-hour support. We work with a wide range of housing and support providers to make sure that this can meet individuals' needs.
Short Breaks. These are available in a residential setting to give family carers a break and provide social opportunities. One of the short breaks services for people with a learning disability moved to a new location in 2023 that was re-developed to be accessible and adaptable. Breaks can range from a couple of days to a few weeks depending on your circumstances.
Please note: Direct payments can also be used if you wanted more flexible short breaks.
Outreach. This support is available to make sure that you can access social opportunities, especially in the evening and at weekends. There are several approved providers who can offer outreach support.
If you or someone you care for have mental health needs
There are various teams that are based in the community that can help you:
Community Mental Health Teams (CMHTs).
- CORE Team - low-level intensive input for people who need support for a short time.
- Enhanced Service - for people with longer-term needs or complex mental ill-health.
Home-Based Treatment Team. Treatment and support for people who are experiencing a mental health crisis in the community to help avoid a hospital admission. The Team also supports people discharged from hospital.
Approved Mental Health Professionals (AMHP) Service. Gives input, advice and Mental Health Act assessments. These are needed after other services have been involved and:
- it is felt that you may not be able to make your own decisions (lack capacity);
- or for your own safety.
There are other services or we can see you at home and link you into activities taking place in your local area. These include:
Share. These are flats where you can stay to:
- relearn skills (this could be after a period in hospital);
- or have a short break to help avoid a relapse or support a carer.
There are also "crisis beds", an alternative to being admitted to hospital and staff are always on the premises.
Union Housing. Offers long-term supported accommodation if you are not able to live independently. There are 17 different properties that offer anything from:
- four people living together in a shared house with staff available on site 24 hours a day;
- to a person living on their own with staff visiting daily.
HOPE Recovery College. For a prospectus, visit: What can we help you with today? The prospectus has a list of courses available. Some of these courses are accessible to anyone in Calderdale and some accessible to just those people supported by mental health services. They are free of charge and they are co-produced with people who have lived experience of mental health needs.
Mental Health Vocational Team. The service can support with the skills you have and work with you to develop new ones that will help you get a job. The staff also support you to apply for jobs, help with interview skills and once you have a job help you to keep that job.
Support for carers
Do you care for a friend, relative or neighbour who would not be able to manage without this help? If so, we can:
- Put you in touch with other carers to offer mutual support.
- Give you information and advice.
- Tell you about services and support groups.
- Do an assessment of your needs.
- Help you set up an emergency back-up plan for the person you care for. (This is in case you are not available for some reason.)
Other organisations that can give specialist support include:
- Carers Count Calderdale. This is a free service to improve the quality of life and wellbeing of local unpaid carers. They offer:
- information and advice;
- drop-in support;
- groups;
- events and activities;
- education;
- benefits and financial advice;
- training;
- and specific support to carers aged 18 to 25.
- Age UK.
We also offer a Carer's Needs Assessment and a Carer's Personal Budgets to eligible carers. This is to support you with your caring role. For more about this, please contact: Carers Count.
There is a range of support groups and activities across Calderdale for carers. These offer the chance to meet other carers and socialise.
Working with others
We work closely with our housing/health partners and local support providers. This makes sure that support you get is joined up and you do not have to keep "telling your story".
Housing services
Heatherstones
This is a Care Quality Commission (CQC) regulated service. It provides temporary accommodation and reablement/therapeutic services if you have been discharged from hospital and:
- are homeless;
- or waiting for adaptations to your property.
There are 11 fully furnished apartments for adults of any age. There are three double apartments on the ground floor that are fully accessible by wheelchair. Couples can stay, you can bring a carer or share with someone else who needs support. The other apartments can be accessed via stairlifts.
This is not a 24-hour service, but each apartment has "telecare equipment", such as fall detectors and access to Progress Lifeline. There are good links with housing services in case you need help with re-housing or adjustments to your home.
Health services
Quest for Quality in Care Homes Service. This operates in 25 older people's nursing and residential homes. It offers support from a team of professionals, such as nurses, pharmacists, consultants and support workers.
It helps residents and staff in a number of ways, such as saving the need to go to your GP.
This was set up to improve quality of care and make sure residents are supported to regain their maximum potential and mobility.
- The service operates weekdays and weekends.
- It can provide direct medical care and advice to prevent the need for GP/hospital care.
Support outside office hours
- Emergency Duty Team. If you have a concern in the evening or at the weekend, please phone: (01422) 288000.
Keeping people safe
Do you feel at risk of or have you experienced abuse? Are you concerned for another adult? If so, phone Gateway: (01422) 393000.
If you become concerned in the evening or at the weekend, phone the Emergency Duty Team: (01422) 288000.
We want to support you to live the life you want, but sometimes things go wrong. At these times, we need to make sure that:
- you are not harmed in any way;
- and the support we give or commission is good quality and safe.
What safeguarding is
It means protecting your right to live in safety, free from abuse and neglect.
It is about working together to support you to make decisions about the risks you face in your life. Also, protecting you if you are not able to make decisions for yourself.
For example:
- Prevent safeguarding issues before they can happen or intervene early to stop things getting worse.
- Set up a Safeguarding Plan to deal with situations where there is risk of abuse or where abuse may have happened.
- Make sure you are not deprived of your liberty without the proper safeguards being in place. (Please see: Mental Capacity and Deprivation of Liberty below).
- Monitor to make sure provision of services are good quality.
- Raise awareness on types of abuse and how safeguarding can help.
In Calderdale, we:
- Always promote your well-being during any safeguarding arrangements.
- Support you to share with us your understanding of safety and how best to identify and achieve your outcomes.
Positive risk-taking
We will support you to take positive risks to enhance your life chances. However, we do make sure people understand the positive and negative outcomes of risk. At times, this means supporting people whose choices may be seen as unwise.
The law says that professionals and other staff should not think that they know best by making people safe without taking account of individual well-being. For more about this, visit: Section 14.8 Care Act - Statutory Guidance (GOV.UK).
Here are some examples of how we would work with people to make sure they are safe in a way that supports their wishes.
Example 1
Mrs Wilson
Mrs Wilson has advanced dementia and lives with her husband who is her main carer. Home carers visit every other day to help Her to have a shower or bath. They have noticed that Mr Wilson has become more short tempered with his wife. The home care workers made a safeguarding alert after he lost his temper with her one morning when she did not want to have a shower. He shouted and became very aggressive with her.
They were visited by a social worker. Mrs Wilson did not recall or understand what had happened. It was clear to the social worker that she still recognised her husband and was very close to him. Mr Wilson was becoming exhausted with providing support to his wife. He explained that this was taking much more time during the night and he was becoming exhausted and irritable. The review of Mrs Wilson's support took into account Mr Wilson's need for some rest and a break from his caring duties. This led to a more suitable support being provided to them that enabled them to stay living together. It also supported Mr Wilson in his role as his wife's carer.
Example 2
Betty
Betty lives on her own and has a care agency visit her four times per day, primarily to support her with her medication and meal preparation. Betty mentioned that her care agency missed a visit one day. A safeguarding concern was raised. Safeguarding staff spoke with Betty to clarify what she would like to happen. Betty responded that this was the first time her care call was missed; she did not miss her medication and got herself a snack and came to no harm.
Betty did not want this raising as a safeguarding concern as she had no other concerns about her care. Staff respected her wishes, but explained they would need to make some enquiries. This was to establish if anyone else may be at risk and to reduce the risk of this happening to others. As the care provider also supported other people.
Safeguarding staff spoke with the care provider. They explained the carer was taken ill on the way to Betty's house. Also, that a substitute could not be found in time for the call as Betty's next call would have been due soon. They had phoned Betty to let her know. No other client calls were missed. They apologised to Betty and this did not appear to be a pattern with the care provider.
The care provider advised safeguarding staff they now had a more robust plan in place should this occur again and Betty was satisfied with actions taken. Betty had the care provider's number added to speed dial so she could call them if needed.
Ways in which we make sure that people are safe
The Mental Capacity Act (MCA) and Deprivation of Liberty Safeguards (DoLS) Team
The law says that no-one should be deprived of their liberty unless this has been through a specific legal process and that they have access to a right of appeal. Anybody who has a high level of care and supervision could be deprived of their liberty in any setting. At home, in a care home/hospital or in supported living.
DoLS is the legal process that Calderdale performs for people living in hospitals and care/nursing homes.
The team:
- Will arrange for you to be seen if you cannot make decisions for yourself because you lack the “mental capacity” to decide where to live and how to be cared for. They will look holistically at your situation and see whether your circumstances and care do appear to reach a point where you are judged to be deprived of your liberty.
- Makes sure that any deprivation of liberty is lawful by completing a total of six independent assessments.
- At least two of these will be done by a Doctor who has had specialist training.
- The rest will be done by a health or social care practitioner who has had specialist training.
- Makes sure that anybody in a care home/hospital who does not have the mental capacity to agree to be there has a representative. Using paid representatives and advocates if needed.
- Makes sure that any care and support is not more restrictive than it needs to be to keep you safe from harm.
For more about this, visit:
See how well we are doing
Making sure that services are of good quality and provided safely
Care Quality Commission (CQC)
The CQC monitors, inspects and regulates care services that we provide or buy from other providers. It visits all regulated care providers and gives a quality rating.
The CQC makes sure health and social care services provide people with safe, effective, compassionate, high-quality care and they, along with the council, encourage care services to improve. These cover:
- Nursing homes.
- Residential care homes.
- Domiciliary care providers (includes supported living).
- Other services in the area.
For the latest regulated services quality ratings in Calderdale services or other parts of the country, visit: Care Quality Commission.
Calderdale Council Quality Team
This team makes sure that registered social care providers meet the quality standards in our Integrated Quality Strategy and Quality Assurance Framework (2023-27). This describes how we work with partners to make sure care and support services are of a good quality. Also, that they meet the needs of people who draw on care and support and that any provider risk is minimised.
Our approach to quality assurance monitoring is undertaken in conjunction with care providers and support is tailored to each organisation’s requirements. The Quality Team assess providers' quality through visits. Also, if necessary, they support the provider to implement an action plan to address any identified areas for development. We also support providers to enhance the quality of life for the people they support, which includes:
- offer new activities;
- and support their staff's well-being.
Comparing our performance with other councils
We do this each quarter with other councils in Yorkshire and Humber and each year with regional and national averages. For more about this, see: Appendix 1 below.
Performance monitoring
We review our performance at our monthly Assurance Board Meetings and where there are areas that we need to improve we set up a story card. This gives us an overview of progress, compares our performance to other councils and describes whether the actions that we are taking are helping to achieve better outcomes for people.
Learning from complaints
We value feedback about the care and support we provide or arrange for you. We know that sometimes things 'go wrong' and we commit to address any issues that later arise.
In the 2024/25 period, we received and looked into 56 complaints (down from 56 in 2023/24).
The resolution times for these were:
- 0 to 15 days: 10.
- 16 to 30 days: 14.
- 31 to 44 days: 3.
Some complaints relate to more than one department or organisation and can take longer to resolve. We let people know if this is going to be the case.
When complaints have been looked into:
- The response is shared with senior managers.
- A log is collated to make sure that we track and analyse the learning. This is to help stop the issue that was found from taking place again.
The themes learned from complaints are shared with staff and managers in our practice forum. Service level and quality was the most common complaint theme in 2024-25. We identify any changes needed to practice or processes and training for staff. These are then put in place and monitored to make sure they are effective.
Our top priorities for next year
To support people to live a 'larger life' we will:
- Strive to improve health and well-being in Calderdale and reduce health inequalities.
- Focus on prevention and early intervention to help people to be better connected in their community and networks.
- Promote equality, diversity and inclusion in everything we do.
- Work in partnership and collaborate with our partners to meet people's needs in a integrated way.
Glossary of Terms and links to more information
Advocacy. Where somebody helps you to express your needs. An advocate would support you or someone you know, to get the social care and support that you might need and they would make sure that your rights are protected.
Assessment. Where a social worker or occupational therapist will have a conversation with you about any social care that you might need.
Care Act (2014). The most recent piece of legislation that councils need to comply with when assessing your needs.
Care Quality Commission (CQC). Monitors, inspects and regulates care services that the council provides or buys from other providers.
Deprivation of Liberty Safeguards (DoLS). Currently applies to people living in hospitals, care homes and nursing homes. The law says that no one should be deprived of their liberty unless this has been done through a process prescribed by law and that they have access to a right of appeal.
Direct Payment. Where the actual money from your Personal Budget is paid to you directly or to someone acting on your behalf, for the cost of arranging all or part of your social care support.
Emergency Duty team. The team that works during the night and at weekends and deals with social care emergencies relating to adults and children. The contact number is 01422 288000.
Extra Care. A group of specially designed apartments which encourage you to be independent. A team based on-site, delivers care and support if you need it, this can be 24 hours. Communal areas also give opportunities to enjoy social activities together, but you still have the privacy of your own apartment.
Gateway to Care. Our information and advice centre. It is a team of Social Care Advisors, Clinical Advisors, Occupational Therapists and Social Workers who can provide you with the information and advice you need to make good decisions about social care.
Lead The Way. An online community advice and support service for adults with learning disabilities or their carers.
Mental Capacity. The ability to make decisions about things like where you live or how you spend your money. The Mental Capacity Act (2005) is there to make sure that people who cannot make these decisions are protected.
Nursing Care. A 24-hour care home where there is always a qualified nurse on duty.
Peer Support. Where support is provided by someone that has had a similar experience to yours.
Personalisation. A way of thinking about care and support services that puts you in control. You say what your needs are and how you would like to have them met. Rather than social care services or providers making assumptions about this.
Personal Budget. The amount of money that is allocated to you by the council to pay for care and support to meet your assessed needs; it gives you much more control in arranging social care to suit your needs.
Pivotal. A round shaped medication prompt dispenser. It is an automatic pill dispenser which reminds you, by means of an alarm and flashing light, when to take your medication. It will make the correct dose available at the correct time of day or night, while keeping other pills locked out of sight.
Reablement. Support that is provided in situations where:
- you might have poor physical or mental health:
- or after a fall or a stroke, to help you to adjust to your situation by learning;
- or re-learning the skills necessary for daily living and to help you to do as much for yourself as possible.
Residential Care. A 24-hour care home that provides help with personal care. There are no nurses available at these homes unlike nursing homes.
Safeguarding. This applies to you if you or someone that you care for:
- Has care and support needs;
- and is experiencing (or is at risk of) abuse or neglect;
- and is unable to protect themselves from either the risk of (or the experience of abuse or neglect) because of those needs.
Social Care. A range of support and advice available from us or other organisations that we can put you in touch with. This is so you can continue to care for yourself, stay safe and live life the way you always have.
Telecare or Assistive Technology. Equipment that helps you to remain safe and independent, in your home, by making links to a monitoring or control centre that can respond to problems as they occur. You press a button on a pendant worn around your neck which alerts someone at the control centre. For example, you need help in an emergency, had a fall, a flood, fire or gas leak. The people in the monitoring centre are trained operators who will arrange for somebody to come and check or alert the emergency services if necessary.
Well-being Plan. A document that you get after an assessment. It sets out the detail of your desired outcomes and how they will be achieved.
What people have told us
Asking people who draw on care and support what they think
From the 2023/24 annual national survey called "The Adult Social Care All User Survey, we found out that:
- The percentage of service users who felt that they had control over their daily life decreased very slightly, dropping from 80.6% in 2022/23 to 79.2% in 2023/24.
- Social contact perception improved for service users for the second year in a row, rising to 51.2% from to 45.5% in 2022/23.
- Overall satisfaction with social care support decreased slightly, falling to 64.5% from 67% in 2022/23.
- A high proportion of service users were able to find out information about services, but there was a slight decrease, falling to 70.6% from 73.% in 2022/23.
- Service users who reported feeling safe remained high at 72.1%, an increase from 71.4% in 2022/23.
Comparing how well we do with other councils regionally and nationally
Each year we send in reports to Government about how well we are doing. Some of this data is included in the national Adult Social Care Outcomes Framework or ASCOF. This is a list of indicators that we can use to compare our performance to other areas or to the national average.
We compare our performance against a group of statistical neighbour local authorities. These are the areas most like Calderdale in relation to their population size and levels of deprivation, as identified by the Chartered Institute of Public Finance and Accountancy (CIPFA). So far, data for 22 ASCOF indicators has been published for 2023/24.
Our performance ranked in the top three for the proportion of
- Carers receiving self-directed support (100%).
- Carers who receive direct payments (100%).
- People who use services who reported that they had as much social contact as they would like (51.2%).
Our performance ranked in the bottom three for:
- Overall satisfaction of carers with social services (25.3%).
- Long term support needs of younger adults (aged 18-64) met by admission to residential and nursing care homes (20.3 per 100,000).
- Proportion of carers who find it easy to find information about services (49%).
For more about our performance, visit: The Adult Social Care Framework (DataWorks).
We monitor our performance regularly and where there are areas that we need to improve we set up a story card. This gives us an overview of progress, compares our performance to other councils and describes whether the actions that we are taking are helping to achieve better outcomes for people.
Sharing our ideas with other councils and learning from them
We work closely with other councils across the Yorkshire and Humberside region on 'sector-led improvement'. This is to make sure that we all provide good quality care and support to people who need it by:
- improving performance;
- sharing ideas;
- and providing support to each other when needed.
Example are:
We are part of the Yorkshire Urban and Rural Social Work Teaching Partnership (YURSWTP). The partnership comprises of:
- Calderdale;
- Kirklees;
- York;
- North Yorkshire Councils;
- Huddersfield;
- York Universities;
- Two NHS trusts:
- Tees, Esk and Wear Valley NHS Trust;
- and South West Yorkshire Partnership NHS Trust.
The partnership works collaboratively to deliver inspirational education and training that leads to high quality social work. The partnership fosters the sharing of good practice to help ensure that social work students are:
- well supported;
- confident;
- and able to practice safely and have a person-centred focus in their placements.
The partnership embraces joint contribution and teaching on curriculums and has successful joint quality assurance processes. By working collaboratively, we aim to:
- grow;
- develop;
- inspire;
- sustain a highly skilled and confident social work workforce;
- and meet the diverse challenges of frontline practice with children and adults.
To make sure we share and learn 'best practice', we are members of regional networks such as:
- safeguarding adults;
- mental health;
- learning disability and autism;
- principal social work;
- and occupational therapy.
How much the council spends on social care support
In 2023/24 we spent £130.9 million on social care services. Every year we have financial pressures, but we managed to stay within our budget, making sure people got the right service (demand management), though we did get some extra money from the Government and the Council.
We provide 30% of all the social care support in Calderdale internally and 85% of our total spend was on care and 15% was on staffing costs.
In 2023/24, our Adults and Wellbeing Directorate had budget savings of £1.1m in year savings to achieve from the gross expenditure budget of £130.9m which it managed to achieve. The Directorate continue to investigate ways of finding ongoing budget savings through Transformation of its services.
The tables below show how the money we spent was broken down by:
- Type of support provided (Table 1).
- Primary reason why people came to us for support (Table 2).
- Type of care provided (Table 3).
Note: Some of the tables below include spend on staffing, so the totals are not the same in them all.
2023/24 Gross Expenditure (per Non-SALT Return on ASC-FR)
| Category of support | Expenditure | % of Spend |
|---|---|---|
| Commissioning and Service Delivery | £8,748,000 | 6.68 |
| Social | £798,000 | 0.61 |
| Assistive Equipment and Technology | £2,716,000 | 2.07 |
| Social Care Activities | £10,301,000 | 7.87 |
| Information and Early Intervention | £1,476,000 | 1.13 |
| Long Term | £102,843,000 | 78.56 |
| Short Term | £4,034,000 | 3.08 |
| Total | £130,916,000 | 100.00 |
(Table 1: Spend by category of support.)
Expenditure by Primary Reason for Support
| Primary reason for support | Expenditure | % of Spend |
|---|---|---|
| Physical | £49,275,000 | 46.10 |
| Sensory | £427,000 | 0.40 |
| Memory and cognition | £6,599,000 | 6.17 |
| Learning disability | £42,572,000 | 39.83 |
| Mental health | £8,005,000 | 7.50 |
| Total | £106,878,000 | 100.00 |
(Table 2: Spend by primary reasons for support.)
Expenditure by Type of Care
| Type of care | Expenditure | % of Spend |
|---|---|---|
| Nursing | £8,508,000 | 7.96 |
| Residential | £34,570,000 | 32.35 |
| Supported accommodation | £1,907,000 | 1.78 |
| Direct Payment | £13,888,000 | 12.99 |
| Home care | £15,457,000 | 14.46 |
| Supported living | £17,749,000 | 16.61 |
| Other long-term | £10,763,000 | 10.07 |
| Maximise Independence | £3,308,000 | 3.10 |
| Other short-term | £729,000 | 0.68 |
| Total | £106,878,000 | 100.00 |
(Table 3: Spend by type of care.)
Tell us what you think
What you think about our services and priorities for the future is important to us. This is so that we can develop the right social care support.
We want to hear from:
- Anyone who has had care and support from us.
- Carers.
- Family members.
- Other people and organisations that have an interest in adult social care.
We specifically would like to know:
- Have we got the balance right in terms of the types of things we think are important?
- Have we set the right priorities?
- Are there other areas of adult care and support that we should be looking at as a potential priority?
- Has the information on this web page been easy for you to understand?
- How can we improve this web page in the future?
Let us know your thoughts about our "Local Account" or to ask us about anything else, contact Gateway to Care:
- Phone: (01422) 393000.
- Email: gatewaytocare@calderdale.gov.uk.
- Website: Contact webform.